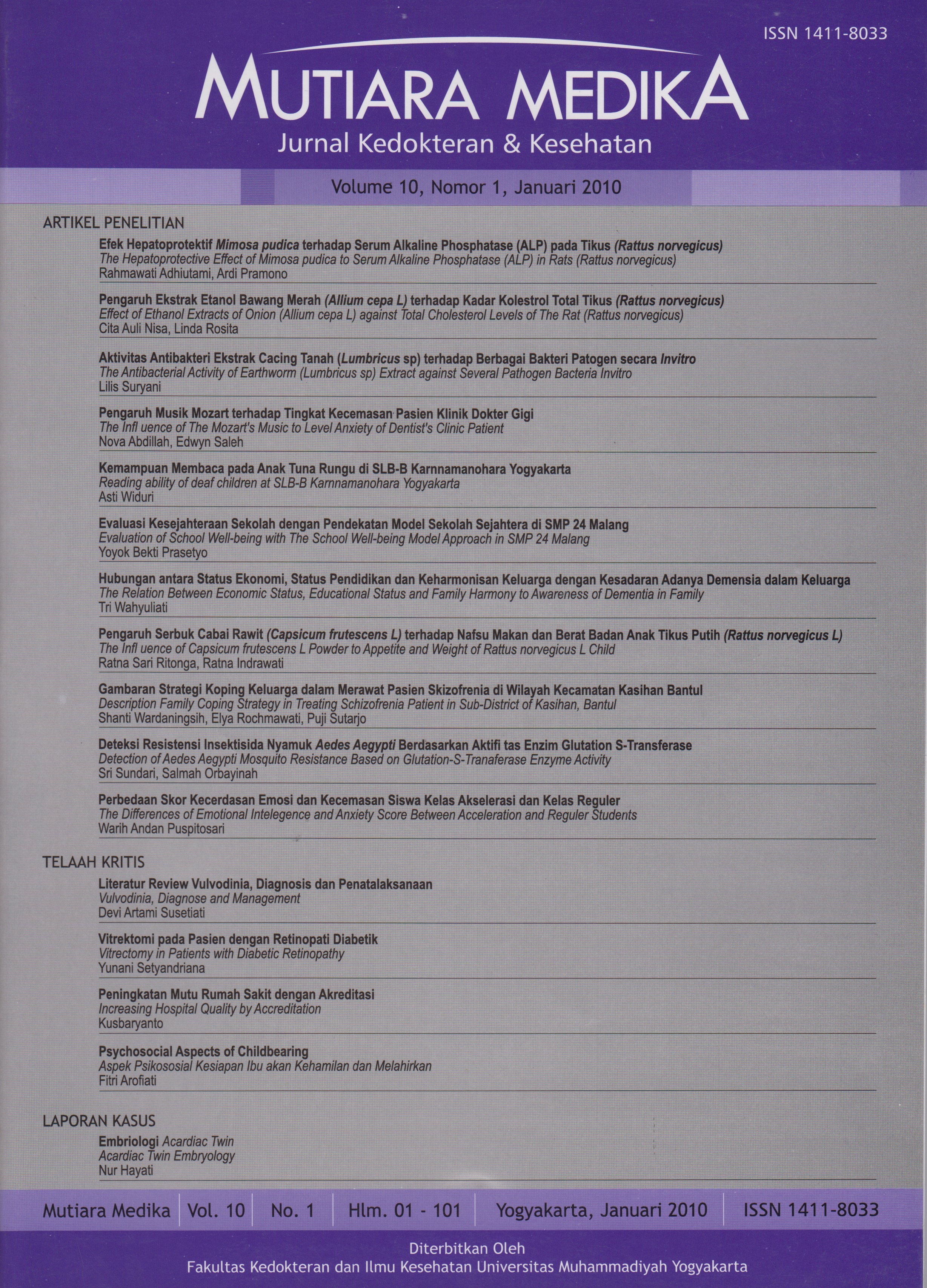
Vitrektomi pada Pasien dengan Retinopati Diabetik
DOI:
https://doi.org/10.18196/mmjkk.v10i1.1566Keywords:
Diabetes Melitus, Retinopati Diabetik, DRVS, IDDM, vitrektomi, Diabetic Retinopathy, vitrectomy, rubeosis iridisAbstract
Retinopathy is a primary morbidity occurring in retinopathy diabetic patients and may cause blindness. The failure of laser treatment to stop the new neovascularization may result in severe vision damage. Vitrectomy is indicated in severe vision patients to improve their vision. The aims of the study were to discuss vitrectomy in diabetic retinopathy patients, refresh the knowledge on how and when Vitrectomy should be performed, and to understand the side effect in order to obtain optimal vision improvement. The method is literature study. Progressive fibrovascular proliferation in diabetic retinopathy patients may lead to retinal detachment. The detachment of posterior retinal without involvement of fovea can be observed. However, if fovea is involved, vitrectomy is indicated. If adequate Laser fails due to media opacity, cataract surgery may be performed. Laser photocoagulation can be conducted a few days postsurgery. Alternatively, both vitrectomy and endolaser may be recommended along with lensectomy and intraocular lens implantation. Diabetic Retinopathy Vitrectomy Study(DRVS) concluded:1) in severe vitreous bleeding eyes, early vitrectomy may result in improved vision despite the high risk of vision loss which needs to be considered.2)In the IDDM patients, especially those with severe vitreous bleeding, early vitrectomy is more beneficial and may have a good result. Postoperative complications may occur including retinal detachment, vitreous bleeding, rubeosis iridis, and other types of complications, which require further considerations for optimal result.The prognosis after vitrectomy depends on the macular function. Surgery for vitreous bleeding without macula detachment generally brings a good result.
Retinopati merupakan penyebab morbiditas utama pada pasien diabetes dengan akibat akhir yang paling ditakuti adalah kebutaan. Kegagalan terapi laser untuk menghentikan proliferasi pembuluh darah baru dapat menyebabkan kerusakan penglihatan yang parah. Pada pasien dengan kerusakan penglihatan yang berat, vitrektomi merupakan terapi yang dapat diharapkan untuk memperbaikinya. Kajian ini membahas tentang vitrektomi pada retinopati DM, menyegarkan pengetahuan kita tentang bagaimana dan kapan vitrektomi dilaksanakan serta mengerti efek yang terjadi supaya didapatkan perbaikan penglihatan yang seoptimal mungkin. Proliferasi fibrovaskular yang progresif pada diabetes dapat mengakibatkan lepasnya retina. Lepasnya bagian posterior tanpa melibatkan fovea dapat tetap stabil dan harus diobservasi, namun begitu fovea terlibat, vitrektomi merupakan indikasi. Jika fotokoagulasi panretinal yang adekuat tidak dapat dilakukan karena opasitas media, pembedahan katarak dapat dilakukan, dan fotokoagulasi laser dapat dilakukan setelah beberapa hari pasca pembedahan. Sebagai alternative, vitrektomi dan endolaser dapat dilakukan bersama dengan lensektomi dengan pemasangan lensa intraocular. Penelitian DRVS menyimpulkan: 1) untuk mata dengan perdarahan vitreus berat, vitrektomi awal menghasilkan tajam penglihatan yang lebih baik, meskipun risiko lebih banyak kehilangan visus sampai tidak didapatkan persepsi cahaya harus dipikirkan. 2) pasien dengan IDDM, khususnya dengan perdarahan vitreus berat, vitrektomi awal lebih menguntungkan dan menghasilkan pemulihan tajam penglihatan yang baik. Komplikasi post operasi dapat terjadi, diantaranya yaitu pelepasan retina, perdarahan vitreus, rubeosis iridis, dan komplikasi lain harus pula dipikirkan lebih lanjut supaya didapatkan hasil yang optimal. Disimpulkan bahwa prognosis penglihatan setelah vitrektomi tergantung pada fungsi macula. Pembedahan untuk perdarahan vitreus tanpa pelepasan macula biasanya menghasilkan ketajaman penglihatan yang baik.
References
Mayfield J. 1998. Diagnosis and Classification of Diabetes Mellitus: New Criteria, American Familly Physician.
Aillo L., Cahill M.M.J. 2001. Systemic Consideration in the Management of Diabetic retinophathy; American Journal of Ophthalmology. 132:760-776
Watkins, Peter J. 2003. ABC of Diabetes Retinophathy: Clinical Review, British Madical Journal. 326:924-926
McCulloch, David K. 2004. Up To Date, Screening for and treatment of diabetic retinopathy. 12;1.
Waspadji, S. 1996. Buku Ajar Ilmu Penyakit Dalam, edisi 3, Jakarta, Balai Penerbit Fakultas Kedokteran Universitas Indonesia.
Guzey, Mustafa, Muftuoglu, Gulipek. 2001. Pars Plana Vitrectomy for High Risk Severe Proliferative Diabetic Retinopathy: Anatomical and Functional Outcomes, Turkish Journal of Endocrinology and Metabolism, 1:31-38
Prasad, S. 2004. Screening for Diabetic Retinopathy: An Overview.
Alberd, Daniel M. 1988. Jakobiec, Frederick A, Robinso. 2004. Principles and Practice of ophthalmology. W.B. Saunders Company; vol.2.
Anonim. 2004. What You Should Know About Diabetic Retinopathy. http:// www.nei.nih.gov.
Anonym. 2004. Eye procedures http:// www.nlm.nih.gov/medicineplus.
Meredith T.A.1994. Current Indications for Diabetic Vitrectomy in medical and Surgical Retina, St. Louis, Mosby, 290¬303
Castelarin, Grigorian, Bhagat, Zarbin. 2003. Vitrectomy with Silicon Oil Infusion in severe diabetic Retinopathy, British Journal of Ophthammology. 87:318-321
Mc Leod. 2003. Silicon oil in Diabetic Vitrectomy. British Journal of Ophthalmology. 87:1300-07
Imamura, Minami, Ueki, Satoh, Ikeda. 2003. Use of Perfluorocarbon liquid during Vitrectomy for severe Proliferative Diabetic Retinopat:563-66
The Diabetic Retinopathy Vitrectomy Study Research Group: Two years course of visual acuity in Severe Prliferative Diaabetic Retinopathy with conventional management. 1985. Diabetic Retinopathy Vitrectomy Study Repord Number 1, Ophthalmology Journal 92:494-502.
Laney J.M., Francis R.R., Kearney J.J. 2003. Combining Phacoemulsification with pars plana Vitrectomy in patiens with Proliferative Diabetic Retinopathy:a series of 223 cases. Ophthalmology 110(7):1335-9.
Afifudin M., Saraswati D.D., Agni A.N. 2005. The Outcome of Vitrectomy in Patients with Diabetic Retinopathy. Proceeding of the 31st Annual meeting Indonesian Ophthalmologist Association. Jakarta.
Bouchard O., Zech J.C., Trepsad C. 1997. Vitrectomy and proliferative Diabetic Retinopathy, J FR Ophthalmol. 20:263-270.
WestJ.F.,GregorZJ.2002.Fibrovascular Ingrowth and Recurrent Hemorrhage Following Diabetic Vitrectomy, British Journal of Ophthalmology. 84:822-825
Helbig, H., Kellner, U., Bornfeld, N., Foester, M.H. 1998. Rubeosis Iridis After Vitrectomy for Diabetic retinopathy, Grafe’Arch clin Exp Ophthalmol.236:730-33
Downloads
Published
Issue
Section
License
Copyright
Authors retain copyright and grant Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK) the right of first publication with the work simultaneously licensed under an Attribution 4.0 International (CC BY 4.0) that allows others to remix, adapt and build upon the work with an acknowledgment of the work's authorship and of the initial publication in Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK).
Authors are permitted to copy and redistribute the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK).
License
Articles published in the Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK) are licensed under an Attribution 4.0 International (CC BY 4.0) license. You are free to:
- Share — copy and redistribute the material in any medium or format.
- Adapt — remix, transform, and build upon the material for any purpose, even commercially.
This license is acceptable for Free Cultural Works. The licensor cannot revoke these freedoms as long as you follow the license terms. Under the following terms:
Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.