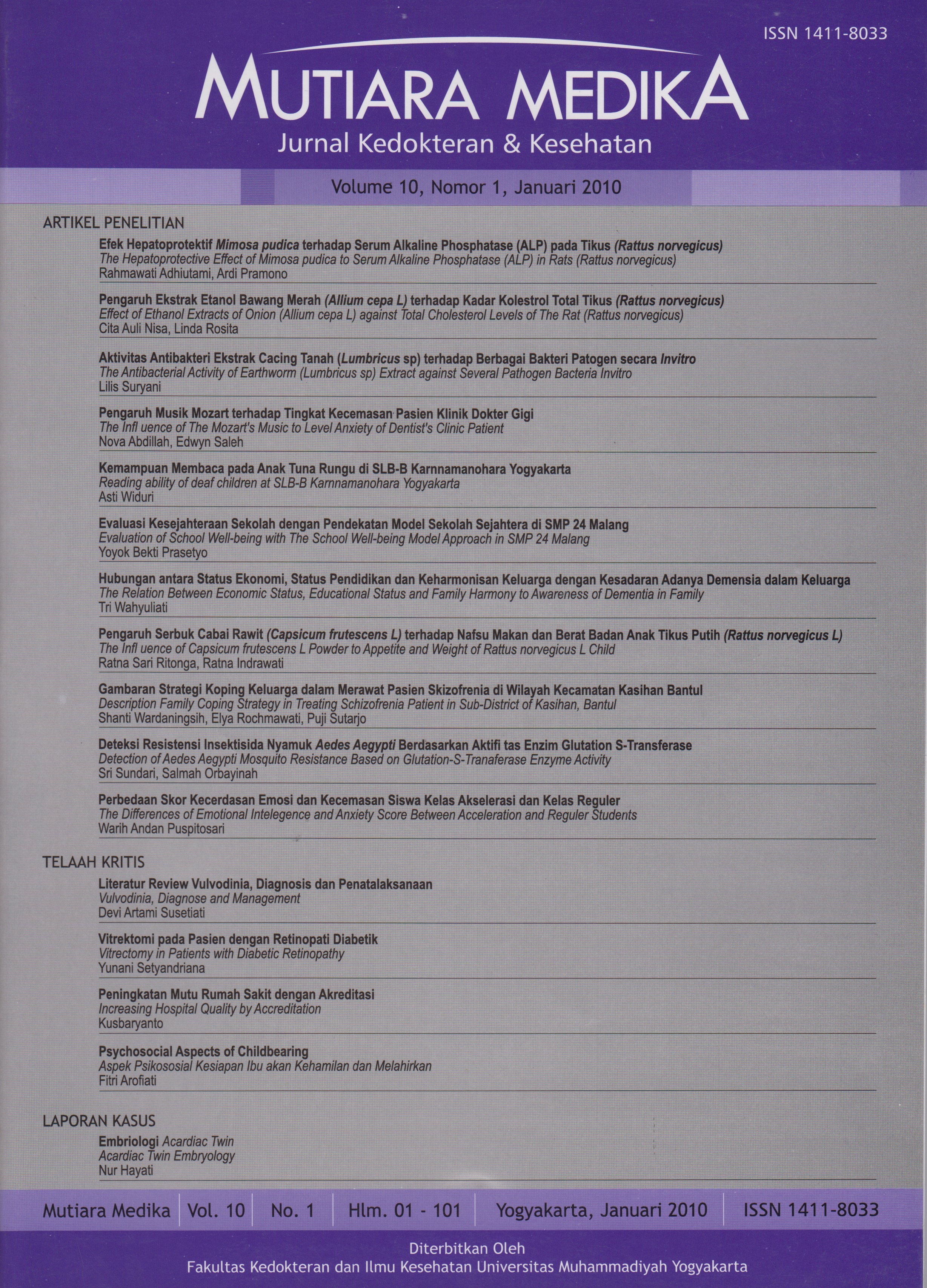
Vulvodinia, Diagnosis dan Penatalaksanaan
DOI:
https://doi.org/10.18196/mmjkk.v10i1.1565Keywords:
diagnosis, manajemen, vulvodinia, diagnose, managementAbstract
Vulvodynia is often described as discomfort or burning pain in the vulvar area, occurring in the absence of visible pathology or a specific, clinically identifiable disorder. The aim of this this article is to give more information about vulvodinia, diagnose and management with literature study method. The diagnosis of vulvodynia is made after taking a careful history, ruling out infectious or dermatologic abnormalities, and eliciting pain in response to light pressure on the labia, introitus, or hymenal remnants. Several treatment options have been used, although the evidence for many of these treatments is incomplete. Treatments include oral medications that decrease nerve hypersensitivity (e.g., tricyclic antidepressants, selective serotonin reuptake inhibitors, anticonvulsants), pelvic floor biofeedback, cognitive behavioral therapy, local treatments, and (rarely) surgery. Most women experience substantial improvement when one or more treatments are used. It can be concluded that vulvodinia ’s management until right now has not been standardized yet because of its etiology.
Vulvodinia merupakan rasa tidak nyaman pada vulva, kebanyakan pasien merasa nyeri terbakar, stinging, iritasi, dan lecet pada daerah tersebut, keluhan berlangsung kronik tanpa disertai gambaran klinis yang spesifik atau gangguan neurologis. Tujuan penulisan makalah ini adalah untuk menambah wawasan tentang vulvodinia, diagnosis dan penatalaksanaannya dengan metode studi pustaka. Diagnosis vulvodinia ditegakkan berdasarkan anamnesis yang teliti dengan menyingkirkan infeksi atau kelainan kulit dan pemeriksaan rasa nyeri terhadap rangsang tekanan ringan pada labia, introitus, atau sisa-sisa himen. Beberapa pilihan terapi telah digunakan meskipun belum cukup terbukti efektivitasnya. Terapi oral dengan menggunakan obat-obatan yang dapat menurunkan hipersensitivitas saraf (misal antidepresan trisiklik, selective serotonin reuptake inhibitors, antikonvulsan), pelvic floor biofeedback, cognitive behavioral therapy, terapi lokal, dan yang jarang dilakukan adalah terapi bedah. Kebanyakan wanita penderita vulvodinia mengalami perbaikan yang berarti ketika menggunakan salah satu atau kombinasi terapi. Disimpulkan bahwa sampai saat ini belum ada standarisasi terapi vulvodinia, hal ini karena vulvodinia merupakan suatu penyakit dengan berbagai kemungkinan etiologi yang belum pasti.
References
Torgerson R.R., Edwards L. 2008. Diseases and Disorders of The Female Genitalia. In Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ. Fitzpatrick’s Dermatology In General Medicine. 7 ed: 675-83.
Goldstein A.T., Burrows L. 2008. Vulvodynia. J Sex Med. 5:5-15.
Reed B.D. 2006. Vulvodynia: Diagnosis and Management. Am. Fam. Physician. 73:1231-38.
Haefner H.K., Collins M.E., Davis G.D., Edwards L., Foster D.C., Hartmann E.H., et al. 2005. The Vulvodynia Guideline. J. Lower Genital Tract Disease. 9:40-51.
Mroczkowski T.F., et al. 1998. Vulvodynia-a Dermatovenereologist’s Perspective. Int J. Dermatol. 37:567-69.
Byth J.L. 1998. Understanding Vulvodynia. Australia. J. Dermatol. 98;39:139-50.
Smart O.C., MacLean A.B. 2003. Vulvodynia. Curr. Opin. Obstet. Gynecol. 15:497-500.
Anonym. 2008. National Vulvodynia Association. www.nva.org. Diakses pada tanggal 16 Juni 2008.
Leppert P., Turner M. 2003. Vulvodynia: Toward Understanding a Pain Syndrome. Proceedings from the Workshop. April 14-15, 2003.
Tympanidis P., Terenghi G., Dowd P. 2003. Increased Innervation of The Vulval Vestibule in Patients with Vulvodynia. Br J. of Dermatol. 148:1021¬27.
Yoon H., Chung W.S., Shim B.S. 2007. Botulinum toxin A for the management of Vulvodynia. Int. J. Impot. Res. 19:84¬87.
Masheb R.M., Lozano C., Richman S., Minkin M.J., Kerns R.D. 2004. On The Reliability and Validity of Physician Ratings for Vulvodynia and The Discriminant Validity of its Subtypes. Pain Medicine. 5:349-58.
Arnold L.D., Bachmann G.A. 2006. Idiopathic Vulvodynia. In: Farage MA, Maibach HI. The Vulva, Anatomy, Physiology, and Pathology. New York, Informa Health Care. 85-97.
Schultz W.W., Basson R., Binik Y., et al. 2005. Women’s Sexual Pain and Its Management. J Sex Med. 2:301-16.
Reed B.D., Caron A.M., Gorenflo D.W., Haefner H.K.. 2006. Treatment of Vulvodynia with Tricyclic Antidepressants: Efficacy and Associated Factors. J. Low. Genit. Tract. Dis. 10:245-51.
Plante A.F., Kamm M.A. 2008. Life Events in Patients with Vulvodynia. BJOG. 115:509-14.
Downloads
Published
Issue
Section
License
Copyright
Authors retain copyright and grant Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK) the right of first publication with the work simultaneously licensed under an Attribution 4.0 International (CC BY 4.0) that allows others to remix, adapt and build upon the work with an acknowledgment of the work's authorship and of the initial publication in Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK).
Authors are permitted to copy and redistribute the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK).
License
Articles published in the Mutiara Medika: Jurnal Kedokteran dan Kesehatan (MMJKK) are licensed under an Attribution 4.0 International (CC BY 4.0) license. You are free to:
- Share — copy and redistribute the material in any medium or format.
- Adapt — remix, transform, and build upon the material for any purpose, even commercially.
This license is acceptable for Free Cultural Works. The licensor cannot revoke these freedoms as long as you follow the license terms. Under the following terms:
Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.